A discussion guide has been developed to help you choose the most appropriate EHC for your customers. It is available here to download and is also available as a tear off pad to ensure you have all the information you need to make the right recommendation.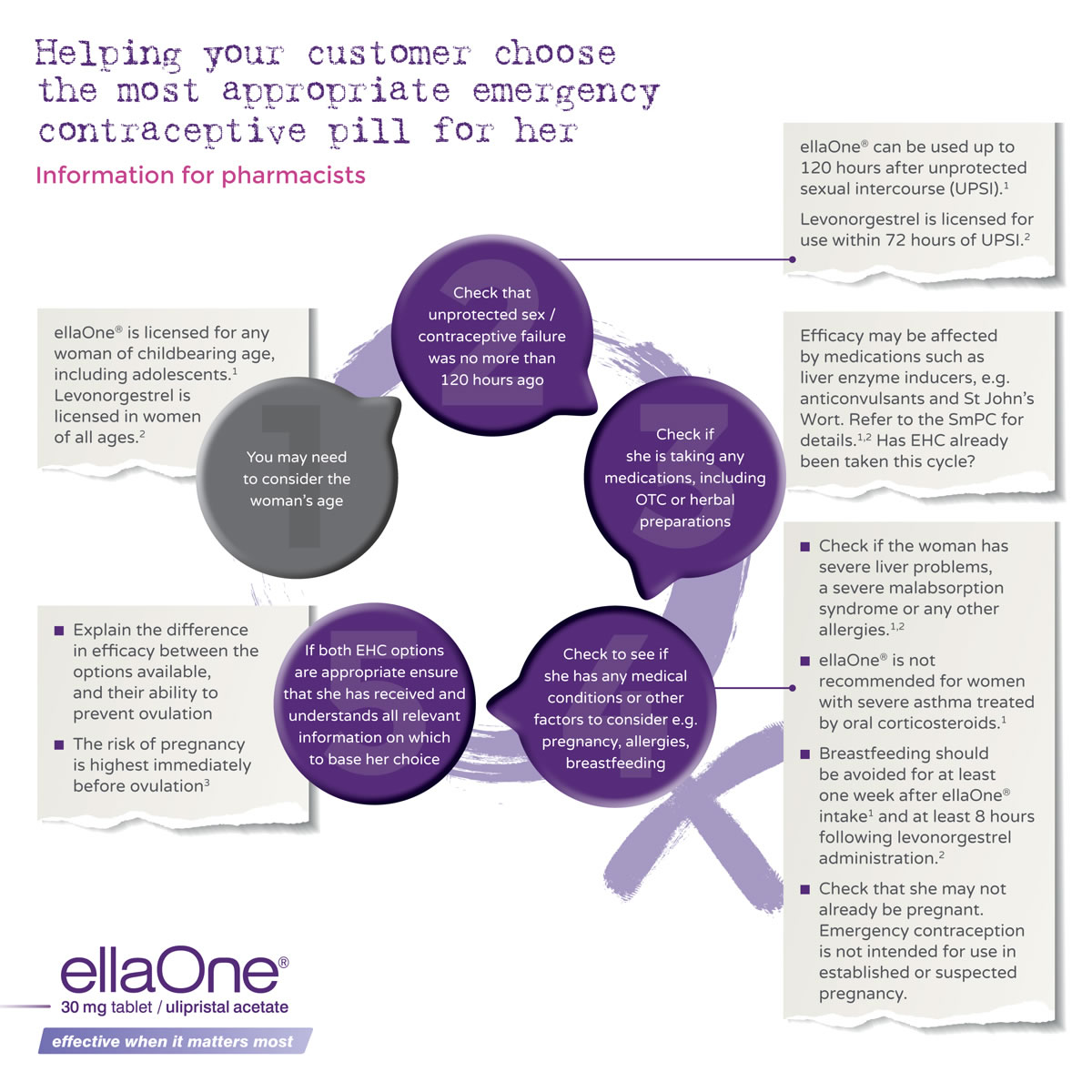
As part of the support for women, we have developed an information leaflet to supplement the PIL. The leaflet is intended to be given to a woman when once it has been decided that ellaOne® is the appropriate product for her. It answers the most commonly asked questions, such as what to do if she vomits, whether further intercourse will be protected, what to expect with her next period and more.
| Step 1: Listen | A woman comes to your pharmacy and asks for the morning after pill. Listen to her needs. Women can download an ellaOne® app, where they can display on their mobile phone screen a request for emergency contraception. They may use this if they are embarrassed to approach the counter when others are around, to request somewhere more private to talk, or that they wish to speak with the pharmacist. Ensure that you and your team are prepared to be approached in this way and be as discreet as possible. |
|---|---|
| Step 2: Reassure |
|
| Step 3: Encourage immediate action |
|
| Step 4: Advise about sex after ellaOne® |
|
| Step 5: Advise what to do if the woman is sick |
|
| Step 6: Advise about the next menstrual period |
|
Pharmacists’ role when providing ellaOne®
Discussing emergency contraception can be distressing for women and it can also be uncomfortable for pharmacists.
You can help by:
- Being matter-of-fact
- Re-assuring them they have done the right thing
- Offering them a more private place to talk if possible (e.g. the consultation room)
- Using customer’s language (referring to the “Morning-after pill” or “Day-after pill” instead of EHC)
- Having a warm and positive approach
You can use the good practice at the counter guide as a framework for your conversation.
Customer satisfaction and comfort in discussing ECPs with a pharmacist can be very high.