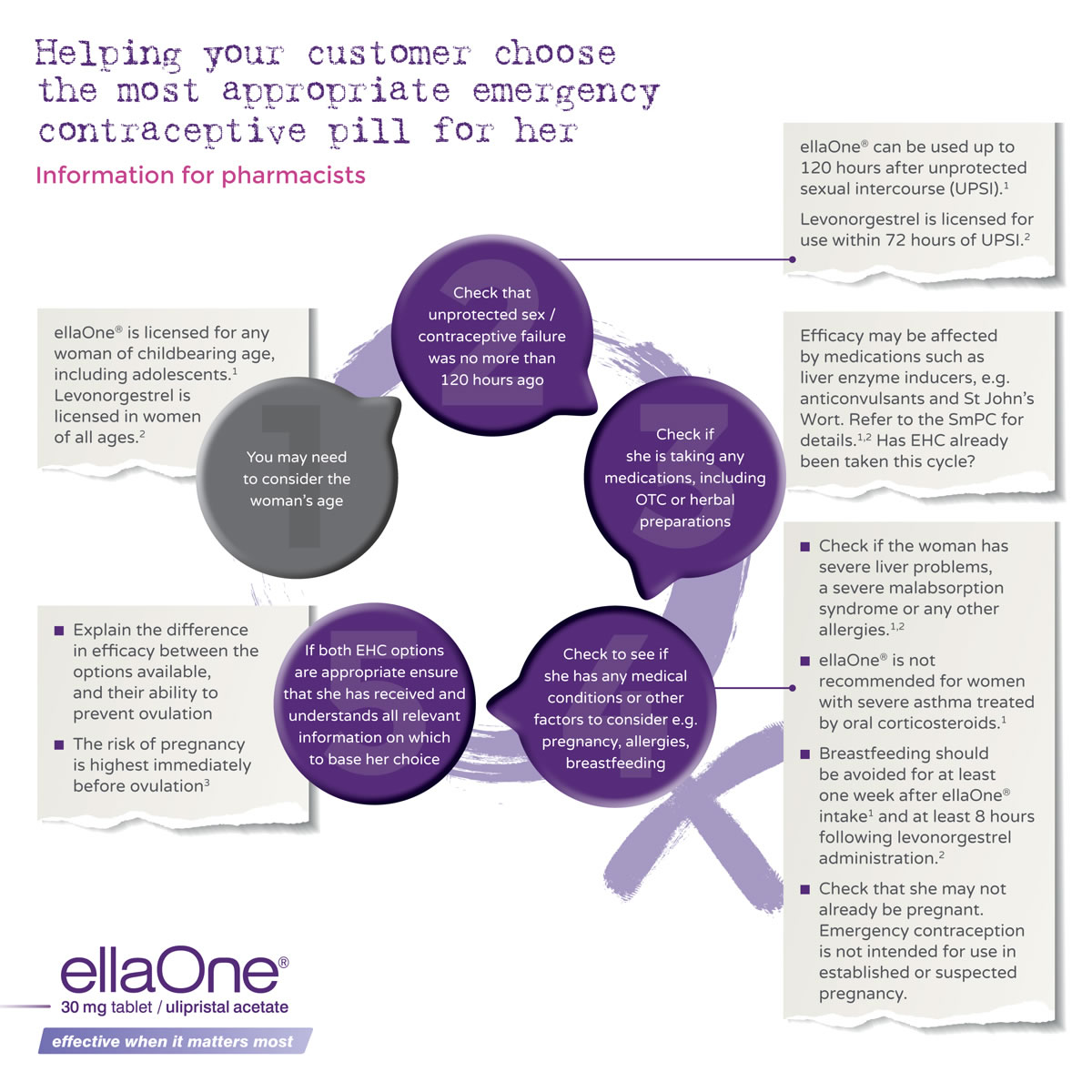
Current emergency contraception solutions are:
- Intrauterine device (IUD), to be fitted in the womb
- Oral emergency contraception, as a tablet
The IUD which is suitable for EC is a Copper-T IUD
IUDs are considered the most effective EC option,1 however they may not be a practical option for many women, as an IUD fitting takes time and involves an invasive procedure by a specifically trained healthcare professional. The advantage of an IUD is that it provides an ongoing contraceptive solution.1 But when speed is of the essence, women may not want to rush a decision to fit this long acting reversible contraceptive (LARC).
The Copper-T IUD can be fitted up to 120 hours (5 days) after unprotected sex.2 Its use is restricted by its availability and the need to be inserted by a skilled healthcare professional.3
Women who would prefer a copper IUD for emergency contraception must be advised to contact a GP or family planning service as a matter of urgency.2 Pharmacists should direct women to a local service known to provide IUDs.2
It is also common practice to consider offering EHC to these women in case there are any problems obtaining or fitting the IUD, or indeed if they change their mind.
There are two oral ECs available4
- One containing levonorgestrel which was first made available in 2005, and became available through pharmacy in 2011.
- One containing ulipristal acetate (ellaOne®), which was launched in 2012.
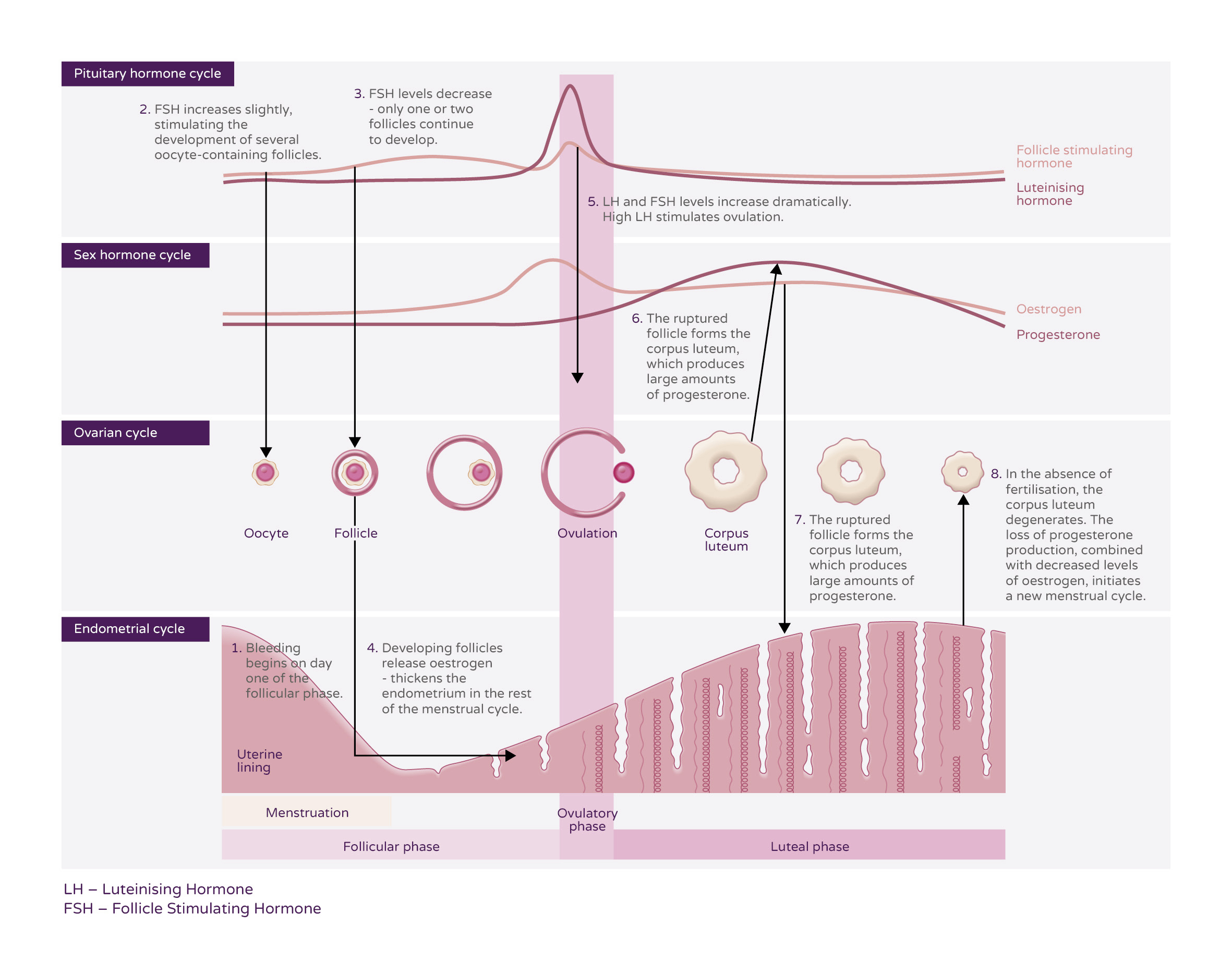
The mechanism of action of oral ECs is to inhibit or postpone ovulation, so that no ovum is released.5,6
Mechanism of action of oral EC
EHCs work by inhibiting or delaying ovulation (the release of an egg), so that fertilisation cannot take place.5,6
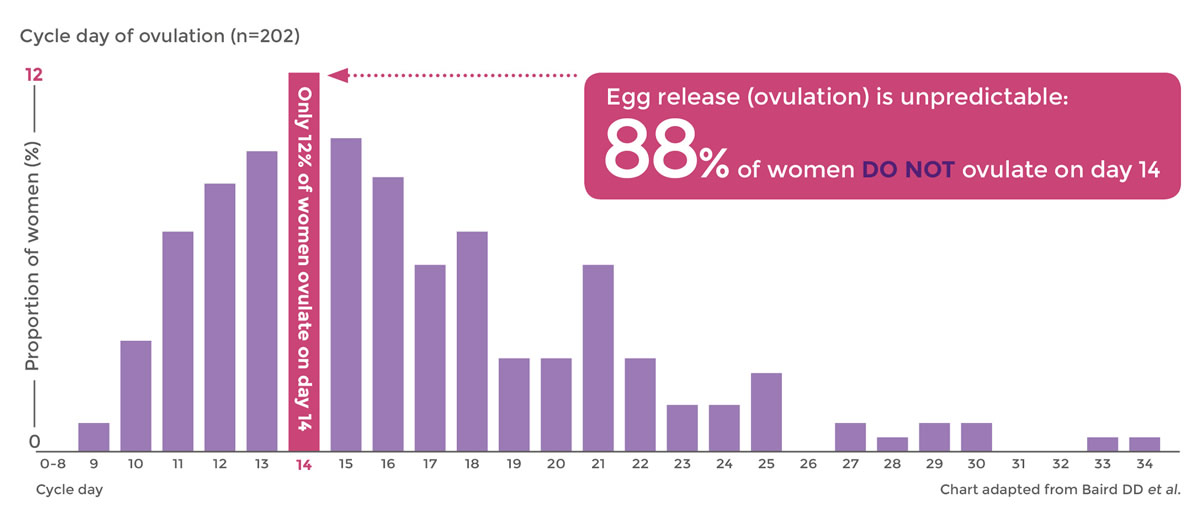
Emergency contraceptive pills will not prevent pregnancy in 100% of cases.5 There is a chance that the woman has already ovulated when she takes an emergency contraceptive pill.7 Taking emergency contraceptive pills as soon as possible after unprotected sex gives the best chance of success.8 EHCs have no effect on fertilisation if ovulation has already happened. They do not interfere with an implanted egg (pregnancy)5,6 so they do not cause abortion8.
EHCs are suitable for women of reproductive age and are generally well tolerated.5,9 EHCs do not protect from sexually transmitted infections (STIs).8
EHCs are back-up contraception solutions, which do not replace a regular contraceptive method.